The COVID-19 Omicron variant has not only led to greater challenges at long-term care centres in 2022, it has also led to greater division among the agencies caring for the most vulnerable.
At the two-year mark of the pandemic, a status update from the operator of four facilities in the greater Edmonton region indicates adaptability has been key to managing through the waves of COVID-19.
“We are better prepared through the lessons learned in 2021,” said John Kopeck, president and CEO of St. Michael's Health Group (SMHG). Kopeck says Omicron outbreaks have occurred at three of the non-profit's facilities, affecting about 15 per cent of the 320-person workforce.
"The majority of cases are being tracked to community; transmission is not happening within our facility," said Kopeck, adding the “strong layer of vaccination that we didn’t have in previous waves” has resulted in fewer severe outcomes. He says outbreaks have been limited thanks to additional rapid testing and screening at the St. Michael's facilities.
Kopeck says SMHG staff is supporting the public health order by not coming to work if they have symptoms, adding "We continue to monitor the situation and are conducting rapid testing on site two to three times per week."
Sandra Azocar, vice-president of the Alberta Union of Provincial Employees (AUPE) which represents 55,000 health care workers in the province, says Omicron outbreaks have been taking a toll on staff and residents across Alberta.
"This poses a serious threat to residents and workers alike. It means longer hours, working without breaks, no time to eat," she said. "After nearly two years in this pandemic, workers were already exhausted, but the scale of the Omicron wave has taken that exhaustion to new levels."
Azocar says appropriate Personal Protective Equipment (PPE) is not always available when needed, and staffing levels are sometimes insufficient.
“We’ve had reports from members that up to half of the normal crew are available on some shifts," she said.
In response, Wayne Morishita, executive director of the Alberta Continuing Care Association--which manages more than 40 per cent of the 28,000 continuing care beds in the province said, “There is no question it has been a challenge managing staffing levels during Omicron but operators have been doing everything they can to provide a high level of care." Morishita says the staffing crunch will be eased when the province’s single site order for continuing care is lifted February 16, allowing people to work at multiple facilities once again.
With respect to PPEs, Morishita said there “was a shortage due to a run on N95s” but that it was corrected quickly.
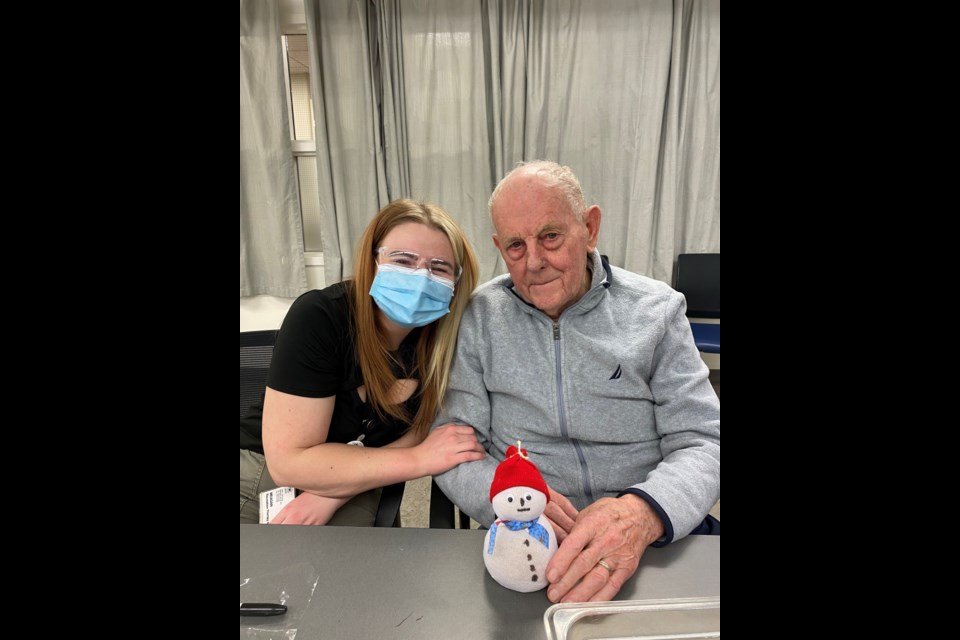
At the St. Michael’s facilities, Kopeck says residents have been coping well and have remained active and enthusiastic.
"We are grateful for the tremendous resiliency, courage, and perseverance shown by our St. Michael’s family, who continue to rise to every challenge of the COVID-19 global crisis in what has been an extraordinary chapter for our organization and in seniors care," he said.
In contrast, Azocar is less optimistic, saying the pandemic has illustrated the need to move all continuing care into the public system.
"Research has shown the level of care provided in facilities that are publicly run is better than in facilities that are privately operated,” she said. “It’s time seniors and others in continuing care are treated the same way we treat others, and we not continue to treat them as second-class users of our health-care system. Unless things change, the future is looking bleak for continuing care in Alberta, both for residents and for workers."
In January, 2022, the federal government introduced new national standards aimed at improving Canada’s long-term care facilities. The recommendations, unveiled by the Health Standards Organization (HSO), are the result of town halls and consultations with Canadians dating back to March 2021. Under the new proposed guidelines, criteria have been added for resident-centred care, safe practices and a healthy, competent workforce.