MONTREAL — A Montreal-based HIV/AIDS research network is expanding its scope in response to a dramatic rise in rates of some sexually transmitted diseases.
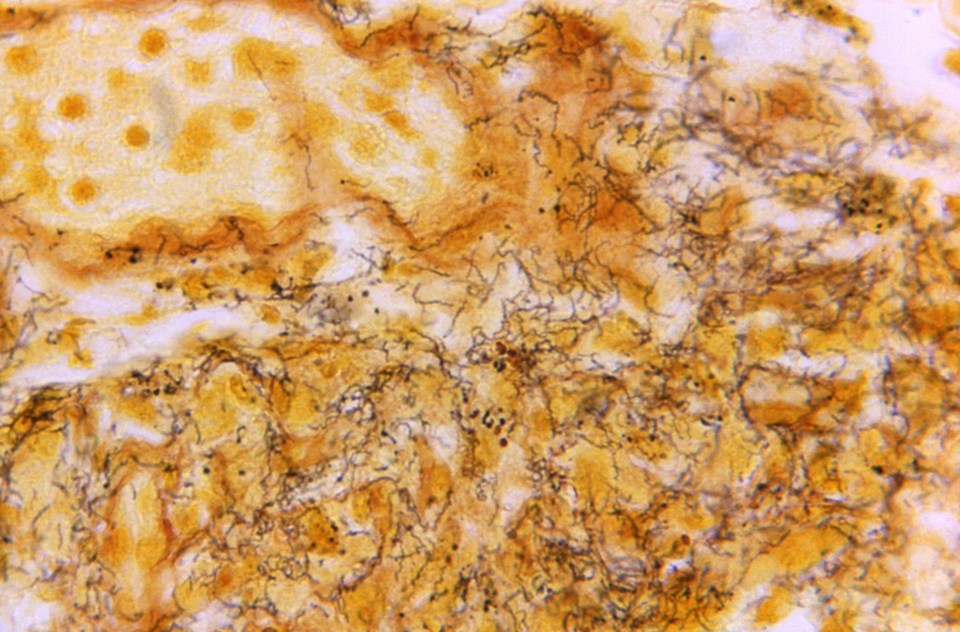
Dr. Marina Klein of the McGill University Health Centre said syphilis rates have increased by more than 100 per cent in recent years across Canada, while HIV diagnoses rose almost 25 per cent between 2021 and 2022. Congenital syphilis — passed down from mother to child during pregnancy — increased 599 per cent between 2018 and 2022, according to the Canadian government.
Klein described the cases of syphilis and other bacterial sexually transmitted infections as "an explosion," adding that the increase in HIV cases is the largest in 10 years.
"In the last several years Canada was making really great strides at meeting the world targets to reduce HIV and other infections, but the COVID pandemic really, I think, derailed some of that," she said.
Klein said the pandemic led to less testing and treatment, but it's not the only reason for the surge. Others include immigration patterns and barriers to accessing care, such as stigma or a lack of health services in certain regions, she said.
"I think that like anything, these issues are complex and probably multifactorial," she said in a phone interview.
She also pointed to the emergence of mpox — formerly called monkeypox — seemingly "out of nowhere" in Canada as an example of how infections themselves can change.
Klein said the Pan-Canadian HIV/AIDS Clinical Trials Network, which was originally formed in 1990, will widen its focus to include all sexually transmitted and blood-borne infections and help find new ways to treat them. The expansion comes after a five-year, $25-million investment from the Canadian Institutes of Health Research, a federal agency.
Klein, who directs the network, said it will help facilitate clinical trials around the country into diseases including mpox, syphilis and hepatitis B. She said projects are already underway to explore preventing sexually transmitted infections in men who have sex with men, as well as testing treatments for mpox.
The resurgence of HIV in Canada is a warning sign that the country can't become complacent, Klein said, adding that as treatments improved and the virus went from a fatal condition to a manageable one, public attention may have shifted.
"It's almost the mindset of, 'OK, we're done with those,'" she said. "And unfortunately that's not the case."
One of the network's goals, she said, is to study prevention and treatment approaches for groups that experience stigma or fear of testing or that may not be able to access consistent care. As an example, she said, Indigenous people, especially in western provinces, have higher rates of HIV and some other diseases than other groups, likely due in part to these barriers.
"Are there things like long-acting therapies that could be administered that could prevent treatment over a long period of time and require less visits to a health professional?" she said. "That's one sort of example of an area we'll be working in."
She said STI rates vary widely across Canada. Klein said the network will offer support to researchers in different regions, especially outside large urban centres, in designing, obtaining approval and funding, and carrying out clinical trials. The network will draw on its many years of experience in HIV/AIDS studies to help researchers run more trials, and to do them better and faster.
After the COVID-19 pandemic, scientists need to be prepared for the emergence of new health threats, she said, adding, "we need to be able to address them in a thoughtful and meaningful way."
This report by The Canadian Press was first published July 17, 2024.
Morgan Lowrie, The Canadian Press